8 Things to Watch For
1. Your “baby blues” don’t get better. It’s common to have a dip in mood during your baby’s first 2 weeks. After that, you should feel better. But if you’re still sad or even hopeless weeks later, and the feelings are growing intense, that’s more than the blues.
2. Sadness or guilt consume your thoughts. Feeling upset once in a while is normal. But if you have frequent crying spells, or you often feel unhappy about being a parent, or you’re often “down on yourself” as a mom, these may be among the first signs of postpartum depression.
3. You lose interest in things you enjoy. Are you laughing at your favorite romantic comedy? Are you interested in being affectionate with your partner? What about your favorite foods? Are you enjoying them? Are you eating at all? If you said no, talk to your doctor about these changes in mood and habits.
4. You have trouble making decisions. Maybe you’re too tired to think straight. Maybe you just don’t care. If you can’t decide whether or not to get out of bed, take a shower, change your baby’s diaper, or take them for a walk, these may be early signs of postpartum depression.
5. You worry you won’t be a good mom. Who hasn’t worried about this? It’s common among moms whose babies are sick or premature, or were born with special needs. But if this is not your situation, then having constant doubts about yourself as a mother could mean something else.
6. Your sleep patterns have changed. Of course, they have. You have a baby! But if you can’t even rest when your child is napping, or you’re sleeping all the time, that’s likely something other than a new sleep pattern.
7. You’ve had big, stressful changes in your life. Maybe you’ve been fighting with your partner, or your family isn’t helping you care for your baby. Perhaps someone you loved died a short time ago. Stressful events like these can worsen your sadness and trigger postpartum depression.
8. You think about harming yourself. Thoughts of suicide, or hurting yourself or your baby, are advanced signs of postpartum depression and even postpartum psychosis, a rare and serious mental illness that happens with postpartum depression. If you’re having any kind of suicidal thoughts, you’re in crisis and need to call your doctor or the National Suicide Prevention Lifeline at 800-273-8255 immediately to get help.
As an MPS, you are NOT qualified or expected to screen moms on calls for postpartum depression but for your own background knowledge and to be well versed in what red flags you may hear in your calls, this information is important to be aware of. Using what you learn about Postpartum Depression (PPD) in your calls with moms could be really helpful as sometimes recognising that you have depression can be extremely difficult but when someone else hears you saying things like “I’m not sleeping even when my baby is because I have insomnia” or “I don’t know what day it is most days” or “I worry constantly that I am not a good mom” you can recognize that they may be in need of more support than just a MPS check-in. Words like “constantly” “always” “never” and “often” are red flags because most emotions and thoughts are not meant to be constant.
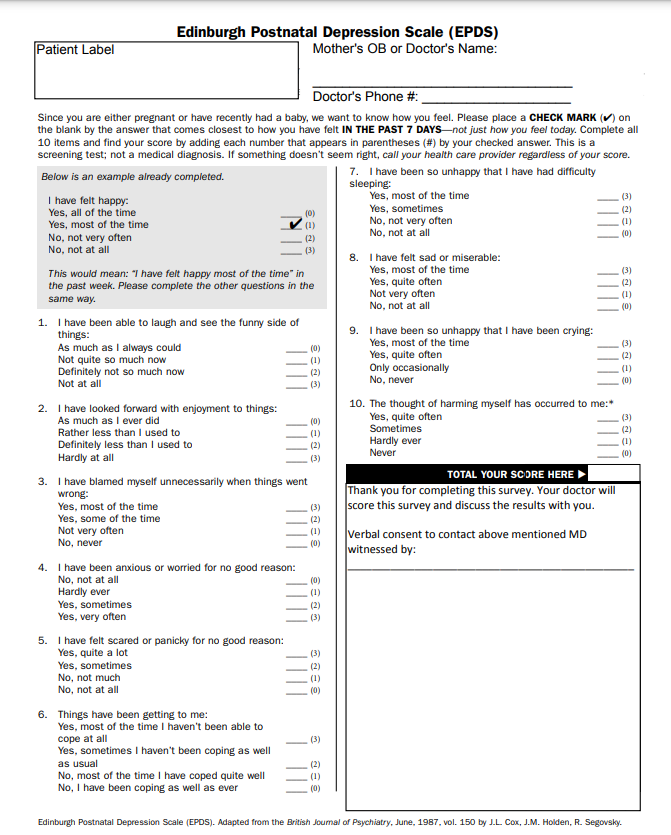
The most commonly used screening tool for PPD (and the industry standard) is called the Edinburgh Postnatal Depression Scale (EPDS). You are NOT asked to perform this screening tool with the moms in your calls but we feel it is important for you to be familiar with it. If you cannot read the image below, the handouts will be available in the “briefcase” portion of the training.